
It is increasingly common for people to own more than one cat. With more than one cat in the home, conflict between cats of the same household is also increasing.
managing aggression in the multi-cat home
It can be challenging to identify aggressive behavior. Cats play roughly and what looks like play might be a fight in progress. Subtle signs like staring and tail twitching are hard to recognize from across the room – overt behaviors such as chasing, wrestling and vocalizing are more likely to catch our eye and ear and alert us to trouble. [Reference 1]
Things to keep an eye/ear out for:
aggression
- vocalizing: growling, hissing, long drawn out meowing
- chasing where one cat is the “chaser”
- offensive postures: stiffened legs, stiff tail
- defensive postures: crouching, tucked head [References 1, 2]
play
- Frequent and long-lasting wrestling/chasing
- You may hear occasional short, soft meows or chirrups [Reference 2]
- Reciprocity – cats take turns being on top or chasing
things in-between
There are interactions that combine both play and aggression but do not result in a fight [Reference 1].
- One cat wants to play and the other does not, responding with a swat and hiss to end the play sequence.
- Cats of different social groups may need to pass each other. There may be some hissing but body postures are not stiff nor crouching.
interventions – Managing Aggression in the multi-cat home
When you hear yowling/hissing/growling or see stiff or crouching postures, it is time to investigate. Intervention may just consist of opening a door wider so that both cats can pass through. If things are a bit more serious, separate the participants using noise or a barrier. See Managing the Indoor Cat Fight.
It is important to identify the social groups in the house. A few aggressive interactions between cats who sleep snuggled together, groom each other and share resources most likely will not require intervention [Reference 1].

PLAY can become AGGRESSION
- A cat becomes too exuberant and begins to scratch and bite harder.
- Reciprocity stops – cats are no longer taking turns.
- Hissing, growling increases as the other cat tries to end the play sequence.
Decreasing aggressive play towards other cats
By reducing the desire to play, cats will play less, decreasing the chance that aggressive play happens [Reference 2].
- Provide play-time for the whole group at predictable times: scatter toys around the room for the group to interact with; play with the aggressive/energetic cats with a wand toy or other interactive toys.
- These more active cats can also benefit from play time away from the other cats in a separate room [Reference 2].
non-play aggression
Play aggression starts with positive, friendly emotions, whereas non-play aggression arises from fear, anxiety, and frustration [Reference 2].
Common scenarios include cats blocking other cats from accessing resources, or trapping another cat in a place that has no escape route. And there are those “bully” cats that “pick on” timid or shy cats, who respond with crouching down and scooting away.
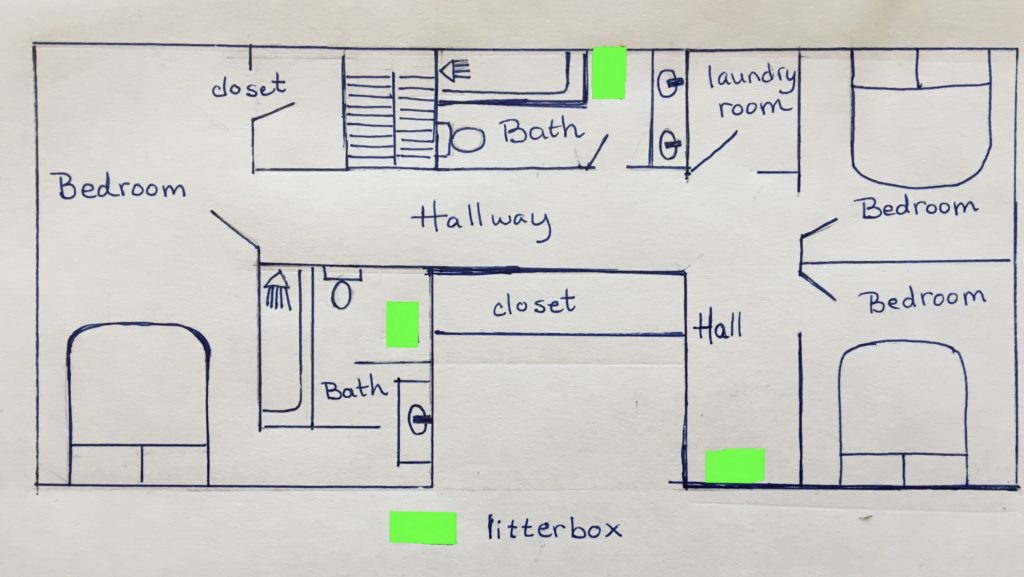
- Have plenty of resources spread out through the house (a cat can’t block two places at once).
- Have multiple, separated play/resting/observation areas.
- Monitor “bottlenecks”: provide places for cats to avoid each other, e.g. a high cat tree near a doorway, offering an escape from another cat passing through.
- Enrich the “bully” cat: give him time away from cats not of his social group with access to food puzzles and novel toys.
- Enrich the “victim”cat: give him or her time away from the bully and his buddies.
- Put a collar with a bell on the “bully” so that other cats know he or she is coming. [Reference 2]
redirected aggression
Something happens that frustrates or frightens a cat, and the cat strikes out at whomever is closest. The cat cannot strike out at the cause of the arousal – it may be out of reach or too risky to confront.
A frequent scenario is a strange cat appearing at a window. The cat indoors cannot engage the stranger and redirects her frustration and anger at another cat nearby. Other triggers include high-pitched or loud noises, unusual odors, or visitors in the house.
Dealing With Redirected Aggression [Reference 2]
- Separate the cats and reintroduce gradually.
- Desensitize the aggressor cat to whatever stimulated the aggression: if it was a noise – play this sound (or something like it) when the cat is around. Start with a low volume and gradually increase to full volume while offering high value treats.
- Visitors in the house: train the cat to go to a safe place when visitors come in.
- For more information, see Redirected Aggression in Your Cat – When It Becomes a Problem.
other interventions – managing aggression in the multi-cat home
- Medication may be helpful for very timid cats, highly aggressive cats, or to manage redirected aggression where the cat will continue to be exposed to the trigger [Reference 2]. See Dealing with Anxiety and Misbehavior in Your Cat.
- If conflict continues, you may need to set up a time-sharing plan and have different social groups use critical areas in shifts. See How Cats Get Along – Timesharing.
- Rehoming the aggressor cat with his social group or the victim cat with her social group may be viable alternatives [Reference 2].
Managing aggression in the multi-cat home requires careful observation of how the resident cats interact with each other. Knowledge of the social groups in the home can help in deciding whether intervention is needed. The cat owner must also be willing to respond to problems by adapting the environment, providing opportunities for cognitive enrichment, such as group and individual play time, and separating and reintroducing cats, when necessary.
Managing aggression in the multi-cat home is essential for the health and happiness of the feline and human occupants.
references
- Gajdoš-Kmecová, N., Peťková, B., Kottferová, J. et al. An ethological analysis of close-contact inter-cat interactions determining if cats are playing, fighting, or something in between. Sci Rep 13, 92 (2023). https://doi.org/10.1038/s41598-022-26121-1
- Ramos D. Common feline problem behaviors: Aggression in multi-cat households. Journal of Feline Medicine and Surgery. 2019;21(3):221-233. doi:10.1177/1098612X19831204









 references
references

 Introducing a new cat to an established group of resident cats can be challenging. Most experts recommend a slow, gradual introduction, similar to how wild cat colonies accept new members.
Introducing a new cat to an established group of resident cats can be challenging. Most experts recommend a slow, gradual introduction, similar to how wild cat colonies accept new members.






