
Saying the final good bye to your cat is never easy. Medical care for cats has progressed by leaps and bounds in the past few decades and it is not uncommon for cats to live to be 19 or 20 years old. As age takes its toll and the older cat’s mind and body declines, many cat owners hope that their old friend will slip away in her sleep. Unfortunately, this does not happen often and we need to decide if it is time for euthanasia.
The word “euthanasia” comes from the Greek: “eu” or well, and thanatos, “death”, i.e. – the good death. A “good death” is the last gift we can give our cats.
The decision to put your cat to sleep is not made lightly.
- The cost of medical care may be out of your reach financially and you elect euthanasia rather than have your cat suffer untreated.
- You may have done all the medical treatments possible and your cat is just not responding. You must say goodbye.
But, what about the cat that clings to survival but is dwindling, still eating but not thriving? When do you say goodbye?
when to say goodbye and put your cat to sleep
In the case of the cat with the “dwindles”, it helps to make a list of what your cat does during her day. Keep an eye on these behaviors and watch for signs of apathy or disinterest.
It can be helpful to keep a calendar of your cat’s daily behavior or events (such as illness or playfulness). Each day can be evaluated as “good”, “bad” or “average”. When the “bad” days outnumber the “good” ones, it may be time to put your cat to sleep. Your veterinarian can help you with assessing your cat’s quality of life.
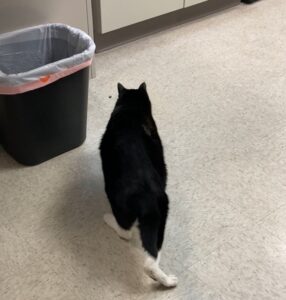
Last week I said goodbye to Marley, one of “The Feline Purrspective” team. Marley was a gentle, extremely sociable cat who enjoyed head rubs and treats. He was friendly with people and fairly tolerant of other cats. His health was generally good until he was about 16 years old. He will be sorely missed.
Marley’s timeline is summarized in the table below. I have highlighted the concerns that contributed to the decision to euthanize.
| AGE | TIMELINE OF LIFE EVENTS |
|---|---|
| 3-14 years |
|
| 14-16 years |
|
| 16-17 years |
|
| 17-18 years |
|
| 18+ years |
|
Looking at the highlighted sections in the table above, you can see that going for walks outdoors and the evening treat/play time were key activities in Marley’s daily life. By the time he is 16-17 years old, he has stopped taking the daily walk but still participates in the nightly treat time. In the next year, he stops this activity.
These behaviors defined who Marley was and were indicators of his will to live. In the final months of his life, he lost this will to live. It was time to say goodbye.
the final goodbye
On February 24, 2024, I said a final goodbye to Marley. I gave him some gabapentin before taking him to the clinic for euthanasia. He passed quickly and peacefully in his basket – he was gone before finishing his favorite treat and before all the euthanasia solution was injected.
The decision to euthanize Marley was based not only on the progression of his medical condition, but also on the changes in his behavior. I feel he was not in pain but his life was no longer worth living. From a friendly, outgoing cat, he had become a reclusive, confused creature, going through the motions of surviving. I don’t feel that his last years were mismanaged but I do feel it may have been kinder to let him go a few months earlier.
I have shared my experience in the hopes that it can help other cat owners who are wrestling with this very difficult question: when to put your cat to sleep. I found it helpful to pay attention to Marley’s daily activities, and note how often he participated in them and when he just stopped doing them. Tracking these key behaviors can give you, the cat owner, an idea of your cat’s mental state: is he is still engaged in life or just going through the motions? If he is just going through the motions, is it time to say goodbye?




 references
references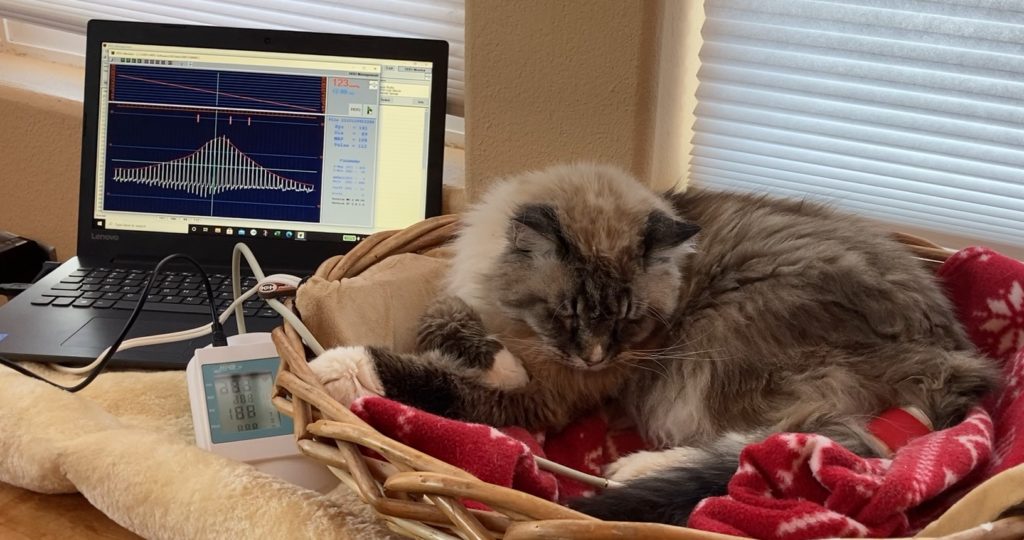

 If you search for “monoclonal antibodies”, most of the search results are about COVID-19 and its variants. But did you know that monoclonal antibodies form the basis of the newest treatment for arthritis in cats? This new treatment is called
If you search for “monoclonal antibodies”, most of the search results are about COVID-19 and its variants. But did you know that monoclonal antibodies form the basis of the newest treatment for arthritis in cats? This new treatment is called 
