
Feline Leukemia (FeLV) and Feline Immunodeficiency Virus (FIV) are among the most common causes of infectious diseases in cats. FeLV can lead to cancer, anemia, and immunosuppression. FIV primarily suppresses the cat’s immune system (Reference 1).
Cats with FeLV and FIV have played a role in human medicine. The discovery of FeLV pointed to the role of viruses in causing cancer. FIV has given us insights into its human counterpart, HIV.
what you need to know about cats with Felv and fiv
Feline leukemia virus (felv)
FeLV was discovered in 1964, when attention was drawn to a multi-cat household with multiple cases of lymphoma. The FeLV virus was found in the cats’ tumors. Once testing procedures were developed in the 1970’s, FeLV was found to be a major cause of disease in owned cats (Reference 2).
FeLV is very infectious. It is passed from cat-to-cat by bodily fluids (Reference 1).
- Infected mother cats shed the virus in their milk and pass it on to their kittens.
- The virus can be found in the saliva, urine and feces of infected cats and can be transmitted by sharing food bowls and litter boxes.
- Cats can also be infected by being bitten by an infected cat.
three stages of FeLV infection (Reference 1).
abortive infection

The cat is able to mount an immune response, killing the virus, and has a lifelong immunity to the virus. These cats will test negative for FeLV but have antibodies to FeLV.
regressive infection
The cat mounts an immune response but does not eliminate the virus. He will become ill with fever, swollen lymph glands, anemia and low white blood cell count. Once recovered, he will be asymptomatic and have antibodies to FeLV but may still have detectable virus in his blood. These cats do not shed the virus in saliva, urine and feces. There is a low chance that the virus may reactivate.
progressive infection
If the cat’s immunity is compromised in some way, her immune response will not be enough to kill the virus. It will spread to the bone marrow and then to the mucous membranes and glandular tissue. The virus is then shed in saliva, urine and feces. Cats with this stage of infection will succumb to cancer or complications of diseases that are usually not fatal.
feline immunodeficieny virus (FIV)
FIV is not as contagious as FeLV. Routes of transmission are (Reference 1):
- Bite wounds that introduce saliva with virus and FIV-infected white blood cells into the wound
- Transmission from queens to kittens is uncommon
- Transmission is uncommon among cats living in households where the cats do not fight
- Unlike humans, sexual transmission is unusual
initial infection with FIV

The cat is ill with fever, swollen lymph glands, and a low white blood cell count.
immune response
The cat’s immune system produces FIV antibodies. The antibodies suppress the amount of circulating virus, lowering the total amount of virus in the infected cat’s blood.
asymptomatic phase
The asymptomatic phase that follows the immune response can last many years, although progressive dysfunction of the immune system can occur. As a result of this deterioration of the immune system,
FIV cats are prone to chronic and recurrent infections.
Cats with FIV are 5 x more likely to get cancer than uninfected cats. However, many FIV+ cats live as long as non-infected cats (Reference 1).
identifying cats with felv and fiv
Identifying and segregating infected cats will help reduce the numbers of cats with FeLV and FIV. The development of Point-of-Care (POC) tests allows the status of cats to be checked when at the veterinary clinic. FeLV vaccines are available to protect uninfected cats.
Screening for FeLV and FIV is recommended (Reference 1) :
- when the cat is first acquired
- prior to vaccination for FeLV
- following exposure to infected cats
- when the cat has clinical signs of illness, eg. dental disease
What is the testing like?
Most POC tests require a few drops of blood from the patient. Results are usually available in 10 minutes. Most test kits include tests for both FeLV and FIV.
Test Results (Reference 1)
Negative Results
- Negative tests are generally reliable
- A retest of a negative result is recommended in 30 days (FeLV) or 60 days (FIV) if there is high risk of recent exposure – for example, a cat bite acquired in a cat fight
- Cats with regressive FeLV infection have low levels of antigen which may not be detected by some tests and the cat will test negative
Positive Results
Because a positive result will involve lifestyle changes, repeat testing is recommended at a reference lab to rule out a “false positive”.
FeLV
- Cats that initially test positive can transition to a regressive infection pattern within 16 weeks of infection.
FIV
- Kittens that nurse on FIV mothers may test positive on a POC test
- Most kittens will test negative once they stop nursing and the maternal antibodies have waned
- Kittens that test positive after 6 months are likely to be FIV+
- Cats vaccinated with FIV vaccines may test positive
vaccines for cats with felv and fiv
FeLV
Vaccines have been developed for FeLV and give cats protection against progressive infections (Reference 1).
Vaccination is particularly recommended for kittens as they are more susceptible to progressive infection than adult cats.
- Kittens can receive their first vaccine when they are 8 weeks or older.
- This first shot is followed by a second dose 3-4 weeks later.
- A booster vaccination is recommended 1 year after the second shot.
- The vaccine may be discontinued for adult cats that are not at risk of interacting with an infected cat (eg. indoor-only)
FIV
FIV vaccination has been discontinued in the US and Canada due to the low protective rate of the vaccine. However, FIV vaccines are still available in other countries, such as Japan, Australia and New Zealand. Cats vaccinated with FIV vaccine may test positive on a POC test (Reference 1).
FeLV and FIV are viruses that together affect 9% of the cat population in North America. These viruses suppress the cat’s immune system making him more susceptible to infections, cancer, and other diseases. POC tests are available to identify cats with FeLV and FIV, allowing cat owners to take steps to protect uninfected cats by vaccination or husbandry. The next post will address caring for virus infected cats and giving them the best of their nine lives.
references
- Little S, Levy J, Hartmann K, et al. 2020 AAFP Feline Retrovirus Testing and Management Guidelines. Journal of Feline Medicine and Surgery. 2020;22(1):5-30. doi:10.1177/1098612X19895940
- Pedersen N, Synopsis of Feline leukemia virus infection and its relationship to feline infectious peritonitis. May 21,2021. https://ccah.vetmed.ucdavis.edu/sites/g/files/dgvnsk4586/files/inline-files/. Viewed January 2024.


 Treating Pandora Syndrome in cats: MEMO
Treating Pandora Syndrome in cats: MEMO










 references
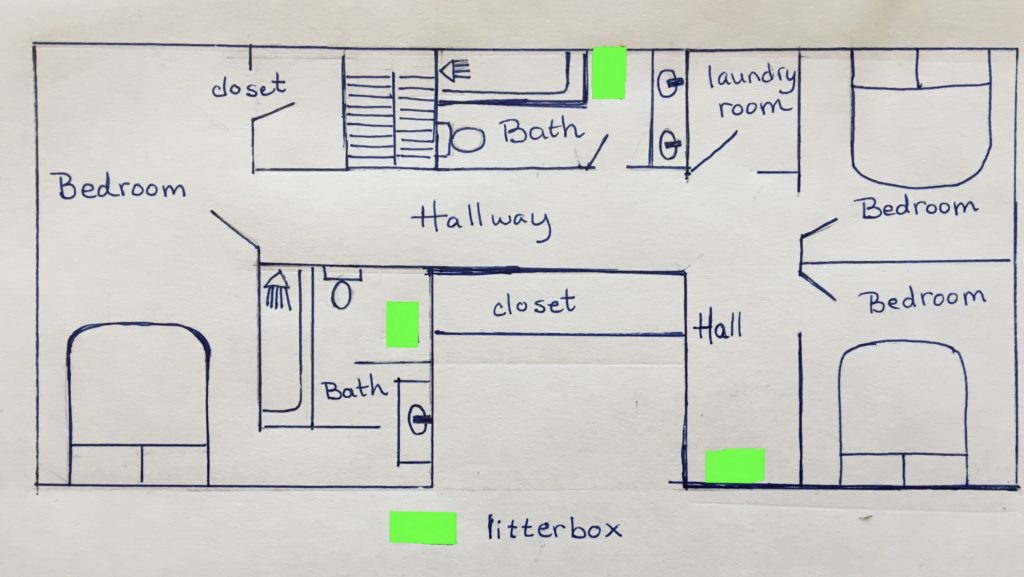
references Introducing a new cat to an established group of resident cats can be challenging. Most experts recommend a slow, gradual introduction, similar to how wild cat colonies accept new members.
Introducing a new cat to an established group of resident cats can be challenging. Most experts recommend a slow, gradual introduction, similar to how wild cat colonies accept new members.



