
Cat ownership is on the rise. The pet food industry sees the cat food market as a place for potential growth. How will trends in the pet food market affect feeding your cat in 2025?
feeding your cat in 2025
How do cats owners choose cat food?
A survey done by the market research company Packaged Facts found that cat owners primarily choose foods that their cats will eat.
- My cat likes it 64%
- I trust the brand 51%
- Price 38%
- Veterinarian recommendation 26%
- packaging nutritional information 25%
(Cats:US Pet Market Trends and Opportunities, 2nd ed. Packaged Facts; September-October 2023 (numbers do not add to 100% as multiple responses were allowed. (Reference 1))
Feeding Your Cat in 2025 – My Cat Likes It
The old dry food stand-by is not as popular with us and our cats these days. Sales of dry cat kibble have dropped from 93% in 2021 to 79% in 2024 (Reference 2).
Cat owners value variety in their cats’ diets and are more likely to feed both canned and dry foods to their pets. Canned cat food sales have increased by several percentage points in the past 2 years (Reference 1). Look for increasing varieties and formats on both canned and dry cat foods.
Feeding your cat in 2025 – health concerns
Fresh Cat Foods
In spite of the limited choice of fresh refrigerated or frozen cat food (products for dogs outnumber those for cats), sales of these foods are increasing as cat owners worry about the healthfulness of highly processed pet foods (Reference 2).
Senior Cats
Senior cat diets may be next in line for an update. Many of these foods were formulated before recent research showed that age-related physiological changes such as immune function and cognitive changes can respond to nutritional intervention (Reference 3).
Energy requirements increase as a cat passes the 12 year mark. Reduced gastrointestinal function, dental disease, and cognitive changes can affect a cat’s food intake. Digestibility becomes paramount. Look for foods designed for senior cats featuring highly digestible protein, increased calories per serving and added supplements including antioxidants, B-vitamins, carnitine, and specific amino acids such as arginine (Reference 4).
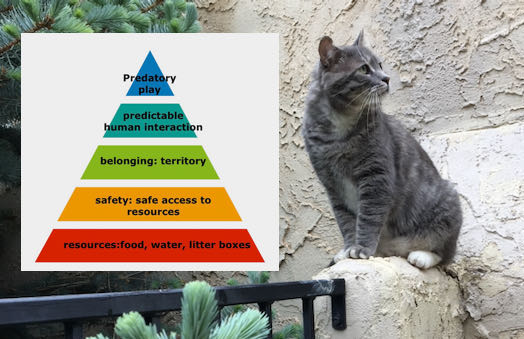
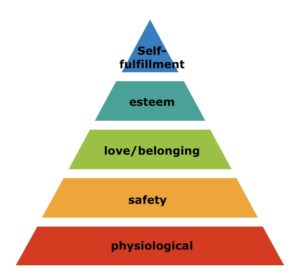
Feeding your cat in 2025 – keep him busy and happy
Cat experts recommend using food puzzles to mimic the foraging behavior of wild cats, keeping the indoor cat busy and portioning out his food. A brief Internet search will turn up a plethora of puzzles and remote feeding systems. Food puzzles range from silicone slow-feeding mats and treat balls the cat rolls around to fleece snuffle mats and puzzles cats have to manipulate to uncover the food.
However, food puzzle use has remained unchanged from 2018 to 2024 – a survey in 2018 (Reference 5) found about 30% of cat owners surveyed used food puzzles; a 2024 survey found that 29% of participants used food puzzles while 21% hid food around the house for the cats to find (Reference 6).
Keep tension low in your household by preventing competition for food. The survey done in 2024 found that most owners (60%) provided the same number of food bowls as cats (Reference 6). Go one step further – give each cat his own food bowl and feed him separately.
Feeding Your Cat in 2025
- Look for high-quality and healthful foods for your cat in 2025. But before you buy, check the food label to see if the food is complete and balanced or just intended for supplemental feeding!
- Replace that bowl of kibble you leave out when you’re gone with some food puzzles.
- Give each cat a separate place at the table.
references
- Landry, Shannon. Why it’s time to pay attention to cats. Pet International Magazine, November 2024, pp. 57-58. https://view.publitas.com/pets-international-1/pets-international-magazine-november-2024/page/58-59
- Phillips-Donaldson, Debbie. Feeding of alternative cat foods rises with cat population. petfoodindustry.com/blogs-columns/adventures-in-pet-food/ February 12, 2025.
- Bermingham EN, Patterson KA, Shoveller AK, Fraser K, Butowski CF, Thomas DG. Nutritional needs and health outcomes of ageing cats and dogs: is it time for updated nutrient guidelines? Anim Front. 2024 Jun 20;14(3):5-16. doi: 10.1093/af/vfae008. PMID: 38910950; PMCID: PMC11188961.
- Molier, Sarah-Jane. Nutritional needs of geriatric cats – time for a change? Pet International Magazine, November 2024, pp. 63-64. https://view.publitas.com/pets-international-1/pets-international-magazine-november-2024/page/63-64
- Delgado M, Bain MJ, Buffington CT. A survey of feeding practices and use of food puzzles in owners of domestic cats. J Feline Med Surg. 2020 Feb;22(2):193-198. doi: 10.1177/1098612X19838080. Epub 2019 Mar 26. PMID: 30912700; PMCID: PMC10814572
- O’Halloran C, Cerna P, Barnicoat R, Caney SM, Gunn-Moore DA. How and why pet cats are fed the way they are: a self-reported owner survey. J Feline Med Surg. 2024 Feb;26(2):1098612X231209894. doi: 10.1177/1098612X231209894. PMID: 38381461; PMCID: PMC10911312.


 Unlike humans, who can place an inhaler between their lips, and breathe the medication in, the coughing cat with asthma, like young human children, must inhale the medication from a chamber.
Unlike humans, who can place an inhaler between their lips, and breathe the medication in, the coughing cat with asthma, like young human children, must inhale the medication from a chamber.


 The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see
The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see 












 references
references