Wild cats have coats patterned with stripes, spots and rosettes, that help them blend in with their surroundings. Cat breeders have crossed wildcats with domestic cats, producing “house” cats with these exotic looks. For a hefty price tag, you can own a wildcat hybrid. But before you reserve your “wildcat”, here are things you need to know.
So you want to own a wild cat hybrid – what you need to know
where do hybrid cats come from?
There are a number of wildcats that can produce hybrid offspring when mated with a domestic cat. The most common hybrids are the Bengal and the Savannah. The Bengal comes from a union of an Asian leopard cat with a domestic cat; the Savannah is the product of the African Serval and a domestic cat (Reference 1).
The offspring of different species are not always fertile – when donkeys and horses are bred together, the results are mules, who are sterile. With wildcats, the first generation (F1) males are often sterile but usually there are some fertile females that can be “bred back” with a domestic male cat. Some of these kittens (F2) may also be sterile and “breeding back” continues until fertility is restored at F4-F5 generations. At this point, the cat is about 15% wildcat (Reference 1).
Usually a female domestic cat is bred to a male wildcat. These unions can have their problems: if the wildcats are not accustomed to domestic cats, they may view the female cat as prey and kill her. Differences in size can pose problems: a male serval can weigh upwards of 20 pounds while the average domestic cat is around 10 pounds. Size will make it physically challenging for the cats to mate (Reference 2).
Successful mating has a better chance with a wildcat who has been raised since kittenhood in a house.
The serval’s gestation period is around 74 days compared with a domestic cat’s 65 day pregnancy. As a consequence, the kittens may be born prematurely, requiring use of incubators to keep them alive.
“Production of hybrid cats promotes illegal trade and removal of exotic cats from their natural habitats for breeding purposes.” (Reference 2) This may threaten the survival of endangered wildcats (Reference 3).
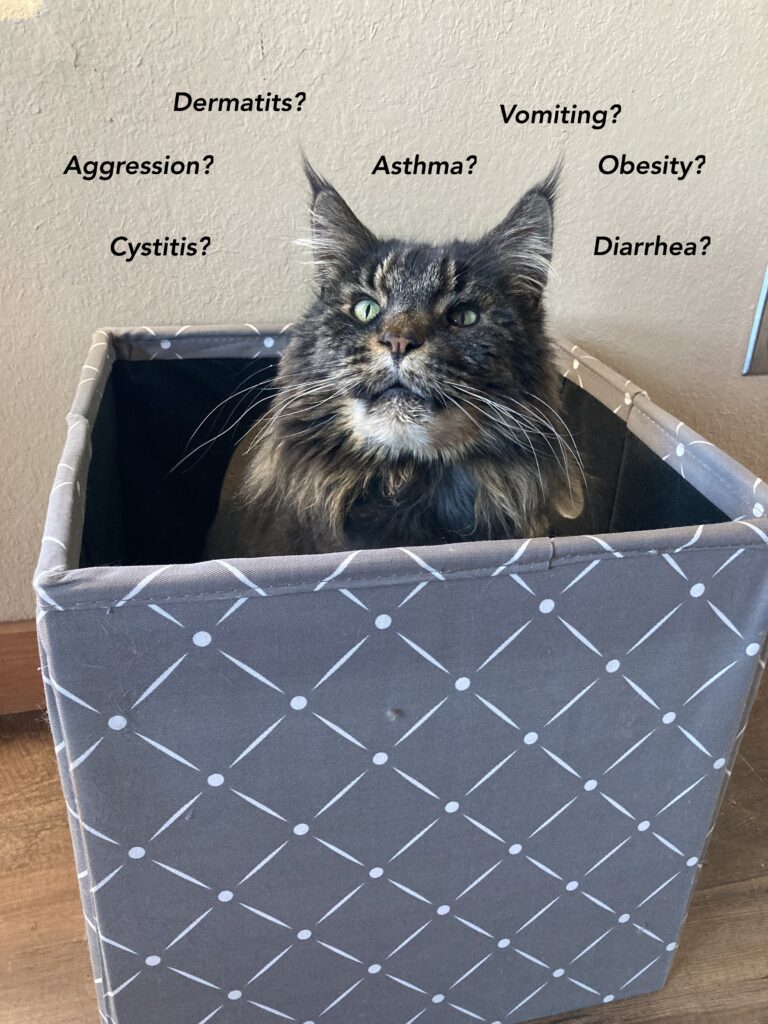
Temperament: something to consider when you own a wildcat hybrid
Domestic cats began their association with humans over 10,000 years ago. There are genetic signatures that identify these cats as domesticated. They have adapted over time from a wild state to close association with humans. In that same time, domestic cats have changed from solitary hunters to more social animals that can live in groups when there is sufficient food.
Wildcats and wildcat hybrids are genetically different than our domestic cat. Temperament is in part influenced by genetics, so it is not surprising that hybrid cats can seem skittish and unpredictable to humans, biting and scratching when not expected (Reference 2). Experts particularly discourage ownership of F1, F2, and F3 wildcat hybrids.
Wildcat hybrids can be more territorial than domestic cats and exhibit behaviors such as urine spraying and aggression toward other pets in the human household (Reference 2).
care and feeding of a wildcat hybrid
Hybrid cats are obligate carnivores like our domestic cats and can be fed a complete and balanced diet of commercial cat food. They may need more calories than the average house cat depending on their size.
Environmental needs are similar to those of our everyday cat although hybrid wildcats can be more active and may need a bit more positive and predictable interaction with people. Leash walking and agility training may be things to consider when you own a wildcat hybrid. Providing a catio can also provide enrichment when you own a wildcat hybrid.
Like any other cat, veterinary care is essential to a long and happy life for hybrid cats. They will need annual exams, vaccinations, and dental care to remain healthy.
The period during which the rabies virus is shed is not known for wild cats so rabies vaccines formulated for a our domestic breeds may not have the same efficacy for hybrids. However, hybrid cats should still receive rabies vaccines (Reference 2).
legal concerns when you own a wildcat hybrid
The locality where you live may require that you have a permit or license to own a wildcat hybrid (Reference 2).
- In Australia and New Zealand, there are complete bans on hybrid cats that are not at least 5 generations removed from a wild ancestor.
- The United Kingdom requires permits for cats with a wild parent.
- Norway and Sweden prohibit cats less than 5 generations removed from a wild ancestor.
- In the United States, laws vary from state to state: Nebraska, Georgia, Hawaii and Rhode Island are the most restrictive.
If your hybrid cat bites a human, local laws may require the cat be euthanized even if vaccinated in order for brain tissue to be evaluated for rabies (Reference 2). In comparison, domestic cats can be quarantined and observed. CHECK YOUR LOCAL LAWS.
When buying a hybrid cat, be aware that a visual exam cannot determine whether a cat is truly an expensive hybrid or a domestic cat with a similar coat color and conformation. To determine authenticity, the breeder should be able to provide a DNA-verified pedigree extending back to the exotic cat foundation (Reference 2).
let the buyer beware…
Hybrid cats are not suitable for the average or first time pet owner.
- They are difficult to breed and costly.
- Hybridization may constitute a threat to endangered wildcat populations.
- These cats can be very active, may seem skittish and unpredictable, and not make good pets.
- Some localities may ban early generations of hybrids; some may require licenses and permits.
The Internet abounds with both horror stories and success stories about wildcat hybrids. Owning a hybrid cat requires an significant investment of not only money, but also time. Like any other cat, exposure to a variety of humans, other pets and household situations when young helps make a good pet. Also, training your hybrid kitten or cat will give him/her a way to communicate with you, accustom him/her to gentle and respectful handling, and strengthen the bond between you and your cat.
An Afterword:
Breeders bred the Asian leopard cat to domestic cats to achieve the distinctive coat of the Bengal cat. In March of 2024, Stanford researchers published a study with the results of 10 years of sequencing the DNA of Bengal cats. They found that the unique appearance of Bengals was a result of variations in genes that had already been present in domestic cats – the beautiful coat of the Bengal cat is NOT due to his Leopard Cat ancestry (Reference 4).
references
- William Murphy, PhD. Genetic Analysis of Feline Interspecies Hybrids, Tufts’ Canine and Feline Breeding and Genetics Conference, 2015
Department of Veterinary Integrative Biosciences, Texas A&M University, College Station, TX, USA https://www.vin.com/apputil/content/defaultadv1.aspx?id=6976361&pid=12513& (viewed 3/2024). - Ownership of non-domestic felids. J Feline Med Surg. 2019 Jul;21(7):NP3. doi: 10.1177/1098612X19857520. PMID: 31234747.
- Devitt, Elizabeth. Mating Game: Survival of Some Small Wildcats At Risk Due to Housecat Hybrids, Mongabay, 5/25/23, https://med.stanford.edu/news/all-news/2024/03/bengal-cats.html (viewed 3/2024).
- Williams, Sarah. Bengal Cat Coats Are Less Wild Than They Look, Genetic Study Finds. Stanford Medicine/New Center/ March 2024. https://med.stanford.edu/news/all-news/2024/03/bengal-cats.html (viewed 3/2024).
Want to keep up with the world of cats? Subscribe to The Feline Purrspective!



 The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see
The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see 






 There has been a stray cat hanging around the house. He is friendly and after a few weeks of feeding him and scratching his head, you decide to adopt him. You do the responsible thing and take him to your vet for an exam, vaccines, and FeLV/FIV test.
There has been a stray cat hanging around the house. He is friendly and after a few weeks of feeding him and scratching his head, you decide to adopt him. You do the responsible thing and take him to your vet for an exam, vaccines, and FeLV/FIV test.





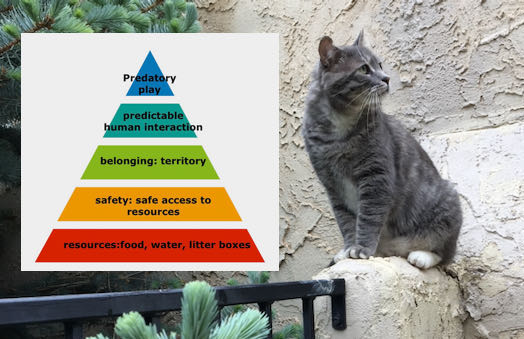
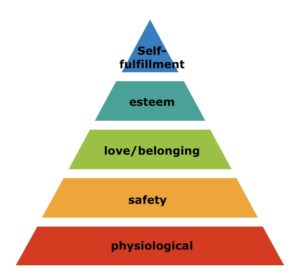
 Treating Pandora Syndrome in cats: MEMO
Treating Pandora Syndrome in cats: MEMO